Cracking down on fraudulent healthcare schemes, U.S. Attorney Jacqueline C. Romero announces a pair of civil settlements totaling nearly $2 million. This duo of settlements is the latest strike in a national push to rein in deceptive billing practices involving the RST Sanexas neoGEN-Series device. For those unfamiliar, the Sanexas device is used to treat pain through electric stimulation, and these particular cases focused on treatments for patients with diabetic neuropathy.
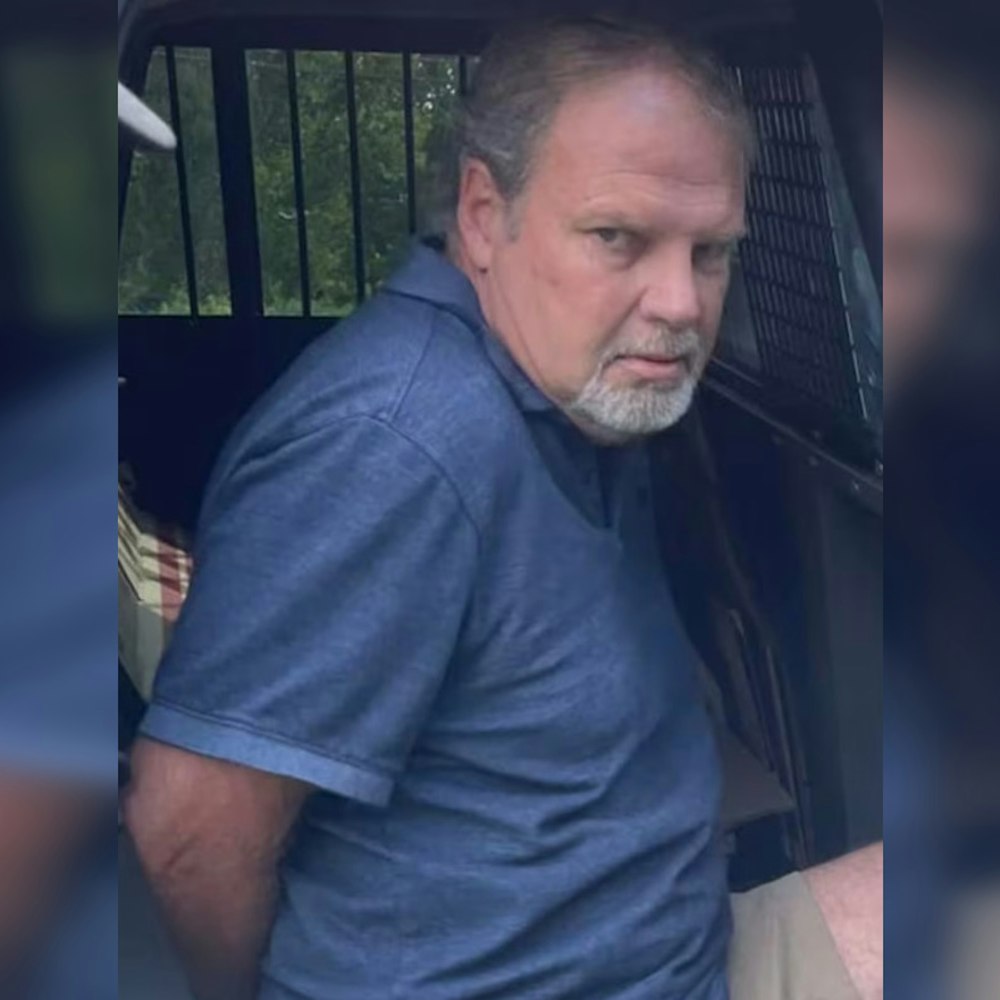
The larger of the two settlements hit Active Integrated Medical Centers, PC, along with its chiropractor co-owners Joseph M. Childs, DC and Charles H. Durr, DC, for $1.9 million. Their crime? Allegedly submitting over 67,000 improper Medicare claims related to Sanexas treatment paired often with vitamin injections. The story takes a twist as Active Integrated apparently refused to cough up the settlement payments, prompting the government to file a complaint to enforce the deal, as reported by the Department of Justice.
On the lighter end of the scale, Nova Integrated Health, PC, run by chiropractor Taylor Vanden Wynboom, DC, agreed to settle for $52,000. This emerged from roughly 33,000 claims to Medicare around the same issue. Wynboom's settlement was reached despite Nova's Chapter 7 bankruptcy declaration, showing the resolve of the U.S. Attorney's Offices from both the Eastern District of Pennsylvania and Southern District of Iowa in pursuing these cases.
At the heart of the problem was a disregard for the specific Medicare coverage limitations for the type of electrical nerve stimulation treatments and vitamin injections used by Active Integrated and Nova. As the DOJ outlined, Medicare does not cover the manner in which the treatments were administered, based on National and Local Coverage Determinations. Additionally, billing codes were allegedly misused — for example, some requiring one-on-one patient contact or mechanical traction — none of which matched the actual service provided.
Beyond the improper use of the Sanexas device and questionable vitamin injections, the clinics also billed Medicare for ENFD testing, a diagnostic procedure to evaluate nerve damage done via a painful skin biopsy, and "TM Flow" testing, which assessed patients' autonomic nervous system and vascular function. Such practices, especially when not medically necessary or used in a manner inconsistent with Medicare's guidelines, are a direct affront to the viability and integrity of the program meant to serve the health needs of the many, not the financial wants of a few.
As the case unfolds, federal health officials continue to send a clear message: due diligence is mandatory and ignorance is no excuse. "Before billing Medicare, providers must conduct their own due diligence, including reviewing applicable coverage determinations; they cannot blindly rely on the advice of device manufacturers, distributors, or billing companies," said U.S. Attorney Romero in a statement. Collaboration between government entities aims to preserve the precious Medicare funds for those in genuine need, rather than losing them to fraudulent and unnecessary claims. The settlements send a stern warning to healthcare providers about the severe repercussions of misleading Medicare billing practices.
-1.webp?w=1000&h=1000&fit=crop&crop:edges)